6 min read
I Was Once Where They Are
“Jesus had been with me through it all; I just didn’t have my eyes open."
5 min read
Lynn Yount, UGM Volunteer
:
March 15, 2017
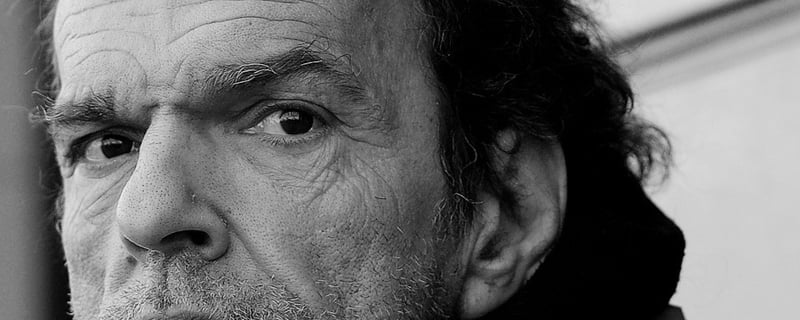
Serious mental illness. It’s a tough topic. But when we exist to serve the homeless, we simply cannot ignore it.
As we mentioned in a previous post, a common estimate is that one-third of homeless people suffer from serious mental illness. A mental illness that is “serious” by definition results in “serious functional impairment, which substantially interferes with or limits one or more major life activities.” (NIMH)
There are too many reasons for this to explore here in depth. Strong correlations between drug abuse and mental illness, family conflict and breakdown from untreated disorders, deinstitutionalization – they all intertwine to fuel homelessness.
So, as a homeless shelter provider, what can Union Gospel Mission do in the difficult cases?
First, we cannot deny it. Some Christians have argued that mental illnesses, and prescribing medications for them, are just worldly descriptions and solutions for spiritual problems. From a certain angle, they have a point: Some spiritual problems can be labeled and medicated by the unbelieving world when the answer to their core problem is in the Gospel.
But just as we trust Christ to be our healer and also take antibiotics for strep throat, there are situations in which faith in Christ’s healing goes hand in hand with using modern medicine to treat a problem in the brain.
“Total depravity means that nothing works as God originally intended. My spiritual desires are affected and distorted by sin. My intellect is distorted by and affected by sin. And, most importantly (for this discussion), my body has been affected and distorted by sin.” (Stephen Altrogge)
In addition to recognizing the problem, we also recognize limitations in the number and type of resources UGM can offer in mental health cases. Men’s Shelter director Gabe Shippam explains that while a majority of the guests are dealing with some kind of mental health issue, none of the staff outside the Recovery Program are mental health professionals, “so we have some big boundaries there.” Overstepping those boundaries and offering opinions about diagnoses and medications can cause more damage than help to those we serve.
That’s why we’re thankful for the help of professionals and agencies in our community that have the expertise and resources to speak to those issues.
While the list of collaborative agencies UGM works with is long, Frontier Behavioral Health is a major partner with UGM’s shelters in Spokane, providing counseling, individual and family therapy, and assistance with medications. In Coeur d’Alene, Heritage Health also plays a strong role in helping our residents get what they need from a medical angle.
 UGM’s role is often in case management and referral, relying on professionals to handle the problems in their purview. Patients can sign a waiver that allows UGM staff and agency staff to discuss their case and help them more effectively. While certified professionals are qualified to diagnose disorders and prescribe drugs, UGM staff can sometimes help them get the most complete picture of a patient’s situation in order to make those decisions.
UGM’s role is often in case management and referral, relying on professionals to handle the problems in their purview. Patients can sign a waiver that allows UGM staff and agency staff to discuss their case and help them more effectively. While certified professionals are qualified to diagnose disorders and prescribe drugs, UGM staff can sometimes help them get the most complete picture of a patient’s situation in order to make those decisions.
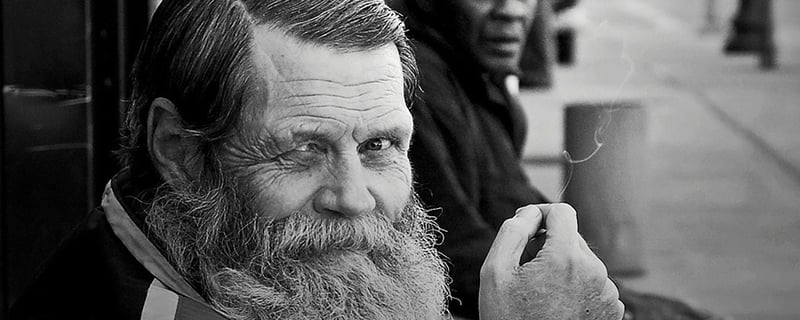
“Because we see them day in and day out, we see a different side of them than their therapist does, because they’re living with us,” Gabe says. “So we actually are able to find a baseline for our clients, and in working with the local agencies, we are able to say, ‘This is really the baseline. He’s functioning down here, or up here.’ ”
To stay at the men’s shelter, “You have to be self-aware and able to manage yourself physically and mentally,” Gabe says. If guests aren’t able to do that, it usually becomes apparent pretty quickly. Men’s Shelter staff are trained in mental health first aid, which helps them recognize and respond to crisis situations with a better understanding of underlying causes. But when people become a threat to themselves or others, staff don’t hesitate to call trained emergency responders.
And while UGM can help people secure their medications, we can’t keep formal schedules to ensure they’re taken properly. Sometimes in severe cases, Frontier staff bring medications to the shelter and make sure the patient takes them on the right schedule.
Mental health care providers are great partners in caring for people who come to UGM, but they have their own boundaries too. They can’t provide the day-to-day relationship and encouragement that are a pillar of how UGM operates.
“We can’t prescribe, we can’t diagnose. But we can walk with someone,” Gabe says.

UGM programs emphasize a “grace-based” environment – meaning rules are enforced at a deeper heart level, compassionately trying to understand the influences and motivations that are causing problems in someone’s mindset or behavior. A secular term that incorporates a lot of the same ideas, Gabe says, is “trauma-informed care.”
Trauma-informed care recognizes that everyone has been through some kind of traumatic experience. Severe trauma in their past is practically a given for people staying in a homeless shelter. That trauma affects the way people cope with situations and shows itself in different ways: sometimes in addictions or in an altered mental state.
“A safe, healing environment that’s relationally driven is a way for that to begin to heal,” Gabe says. That’s why UGM is protective of its clean and sober shelters. It’s important for guests to have consistency and protection as they deal with disorders that have been years in the making.
UGM uses a scale of zero to 5 to assess various areas of a guest’s situation – in the housing category, for example, a zero would mean someone is chronically homeless on the streets, while a 5 would mean living in permanent housing without subsidies.
We would love for everyone to hit the 5 on that scale. But in the area of mental disorders, it’s important to recognize the smaller steps forward as success, so we don’t use those kinds of simplified measurements.
One guest Gabe uses as an example is a guest who is about 70, who has had to go to the hospital before because of his disorder. But he comes back to the shelter when he’s stabilized. He actually likes living at UGM, but staff realize the best they probably can do for him is to find the type of skilled residential facility that can handle his care, then “push him out of the nest” and make sure he understands he will be safe and cared for there.
That gentleman has certainly improved while a guest of UGM. But he’s unlikely to be moving out on his own and completely managing his own health. Does that mean we would have failed in caring for him?
 Another way to change how we think about success: Some guests have claimed God has healed them of their disorder, so they quit their psychiatric medications cold turkey or quit trying to learn the coping skills by which most people manage mental illness. They assume the struggle is over.
Another way to change how we think about success: Some guests have claimed God has healed them of their disorder, so they quit their psychiatric medications cold turkey or quit trying to learn the coping skills by which most people manage mental illness. They assume the struggle is over.
One gentleman claimed to be healed of his disorders and stopped taking his medication. A while after he left the shelter, Gabe says, “I ran into him in a different part of town and he was out of it. Didn’t know who he was or what he was doing. It wasn’t because of substance abuse; it was because of substance neglect.”
While we fully believe in God’s ability to heal any disease or disorder however he wills, most of the time he does it through careful treatment and management. Someone being faithful and disciplined to trust him to work over a longer period of time, and endure some difficulty along the way, is usually a more successful outcome than an instant “healing” that may be an illusion. When people’s minds are cleared, “unoccupied, swept, and put in order,” they must be filled with Jesus and guarded so that the “unclean spirit” that was removed doesn’t just return with a vengeance (Matthew 12:43-45).
So UGM continues to see each person as an individual, with varying needs, strengths and weaknesses, who needs God’s mercy just as we all do. We share the good news of his grace, of the power of Jesus and the cross. We focus on doing what we can do with excellence.
Phil Altmeyer shares some of the lessons he's learned in three-plus decades of working with the poor and homeless in this free e-book.

6 min read
“Jesus had been with me through it all; I just didn’t have my eyes open."

2 min read
“Let us hold unswervingly to the hope we profess, for He Who promised is faithful…Jesus Christ is the same yesterday, today, and forever.” (Hebrews...

9 min read
To celebrate 75 years of serving the Inland Northwest, we are spending the year remembering our history and the faithfulness that built us and...

1 min read
Editor’s note: Recently we’ve been talking about mental struggles on the Impact Blog. From insomnia to trauma and addiction, there are many struggles...

It’s hard to talk about homelessness without talking about mental illness. An oft-quoted estimate suggests that as many as one-third of homeless...

We talked about trauma recovery and why it’s important for people like Jocelyne in July’s Mission News. On one hand, it’s complicated: family...